What is Atrial fibrillation?

Overview
Atrial fibrillation is an irregular and often rapid heart rate that commonly causes poor blood flow to the body.
During atrial fibrillation, the heart's two upper chambers (the atria) beat chaotically and irregularly — out of coordination with the two lower chambers (the ventricles) of the heart. Atrial fibrillation symptoms often include heart palpitations, shortness of breath, and weakness.
Episodes of atrial fibrillation can come and go, or you may develop atrial fibrillation that doesn't go away and may require treatment. Although atrial fibrillation itself usually isn't life-threatening, it is a serious medical condition that sometimes requires emergency treatment. It can lead to complications. Atrial fibrillation may lead to blood clots forming in the heart that may circulate to other organs and lead to blocked blood flow (ischemia).
Treatments for atrial fibrillation may include medications and other interventions to try to alter the heart's electrical system.
People also search: What is A fib?

Symptoms of Atrial fibrillation
A heart in atrial fibrillation doesn't beat efficiently. It may not be able to pump enough blood out to your body with each heartbeat.
Some people with atrial fibrillation have no symptoms and are unaware of their condition until it's discovered during a physical examination. Those who do have atrial fibrillation symptoms may experience signs and symptoms such as:
- Palpitations, which are sensations of a racing, uncomfortable, irregular heartbeat or a flip-flopping in your chest
- Weakness
- Reduced ability to exercise
- Fatigue
- Lightheadedness
- Dizziness
- Confusion
- Shortness of breath
- Chest pain
Atrial fibrillation may be:
- Occasional: In this case, it's called paroxysmal (par-ok-SIZ-mul) atrial fibrillation. You may have symptoms that come and go, lasting for a few minutes to hours and then stopping on their own.
- Persistent: With this type of atrial fibrillation, your heart rhythm doesn't go back to normal on its own. If you have persistent atrial fibrillation, you'll need treatment such as an electrical Shock or medications in order to restore your heart rhythm.
- Permanent: In this type of atrial fibrillation, the normal heart rhythm can't be restored. You'll have atrial fibrillation permanently, and you'll often require medications to control your heart rate. Most people with permanent atrial fibrillation will require blood thinners to prevent blood clots.
When to see a doctor
If you have any symptoms of atrial fibrillation, make an appointment with your doctor. Your doctor may order an electrocardiogram to determine if your symptoms are related to atrial fibrillation or another heart rhythm disorder (arrhythmia).
If you have Chest pain, seek emergency medical assistance immediately. Chest pain could signal that you're having a Heart attack.
Causes of Atrial fibrillation
Atrial fibrillation is an irregular and often rapid heart rate that occurs when the two upper chambers of your heart (atria) experience chaotic electrical signals.
Your heart consists of four chambers — two upper chambers (atria) and two lower chambers (ventricles). Within the upper right chamber of your heart (right atrium) is a group of cells called the sinus node. This is your heart's natural pacemaker. The sinus node produces the impulse that normally starts each heartbeat.
Normally, the impulse travels first through the atria and then through a connecting pathway between the upper and lower chambers of your heart called the atrioventricular (AV) node. As the signal passes from the sinus node through the atria, they contract, pumping blood from your atria into the ventricles below. As the signal passes through the AV node to the ventricles, it signals the ventricles to contract, pumping blood out to your body.
In atrial fibrillation, the upper chambers of your heart (atria) experience chaotic electrical signals. As a result, they quiver. The AV node — the electrical connection between the atria and the ventricles — is bombarded with impulses trying to get through to the ventricles. The ventricles also beat rapidly, but not as rapidly as the atria, as not all the impulses get through. The reason is that the AV node is like a highway on-ramp — only so many vehicles can get on at one time.
The result is a fast and irregular heart rhythm. The heart rate in atrial fibrillation may range from 100 to 175 beats a minute. The normal range for a heart rate is 60 to 100 beats a minute.
Possible causes of atrial fibrillation
Abnormalities or damage to the heart's structure is the most common cause of atrial fibrillation. Possible causes of atrial fibrillation include:
- High blood pressure
- Heart attacks
- Coronary artery disease
- Abnormal heart valves
- Heart defects you're born with (congenital)
- An overactive thyroid gland or other metabolic imbalance
- Exposure to stimulants, such as medications, caffeine or tobacco, or alcohol
- Sick sinus syndrome — improper functioning of the heart's natural pacemaker
- Lung diseases
- Previous heart surgery
- Viral infections
- Stress due to Pneumonia, surgery, or other illnesses
- Sleep apnea
However, some people who have atrial fibrillation don't have any heart defects or damage, a condition called lone atrial fibrillation. In lone atrial fibrillation, the cause is often unclear, and serious complications are rare.
Atrial flutter
Atrial flutter is similar to atrial fibrillation, but the rhythm in your atria is more organized and less chaotic than the abnormal patterns common with atrial fibrillation. Sometimes you may have Atrial flutter that develops into atrial fibrillation and vice versa.
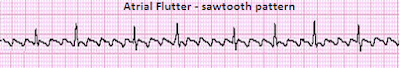
The risk factors for and the symptoms and causes of Atrial flutter are similar to those of atrial fibrillation. For example, Strokes are also a concern in someone with Atrial flutter. As with atrial fibrillation, atrial flutter is usually not life-threatening when it's properly treated.
Risk Factors
Certain factors may increase your risk of developing atrial fibrillation.
These include:
- Age. The older you are, the greater your risk of developing atrial fibrillation.
- Heart disease. Anyone with Heart disease — such as heart valve problems, congenital Heart disease, congestive Heart failure, Coronary artery disease, or a history of Heart attack or heart surgery — has an increased risk of atrial fibrillation.
- High blood pressure. Having high blood pressure, especially if it's not well-controlled with lifestyle changes or medications, can increase your risk of atrial fibrillation.
- Other chronic conditions. People with certain chronic conditions such as thyroid problems, Sleep apnea, Metabolic syndrome, Diabetes, Chronic kidney disease or lung disease have an increased risk of atrial fibrillation.
- Drinking alcohol. For some people, drinking alcohol can trigger an episode of atrial fibrillation. Binge drinking may put you at an even higher risk.
- Obesity. People who are obese are at higher risk of developing atrial fibrillation.
- Family history. An increased risk of atrial fibrillation is present in some families.
Complications
Sometimes atrial fibrillation can lead to the following complications:
- Stroke. In atrial fibrillation, the chaotic rhythm may cause blood to pool in your heart's upper chambers (atria) and form clots. If a blood clot forms, it could dislodge from your heart and travel to your brain. There it might block blood flow, causing a Stroke.
- Heart failure. Atrial fibrillation, especially if not controlled, may weaken the heart and lead to Heart failure — a condition in which your heart can't circulate enough blood to meet your body's needs.
Preparing for Your Appointment
If you think you may have atrial fibrillation, it is critical that you make an appointment with your family doctor. If atrial fibrillation is found early, your treatment may be easier and more effective. However, you may be referred to a doctor trained in heart conditions (cardiologist).
Because appointments can be brief, and because there's often a lot to discuss, it's a good idea to be prepared for your appointment. Here's some information to help you get ready for your appointment, and what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your dietary intake. You may need to do this if your doctor orders blood tests.
- Write down any symptoms you're experiencing, including any that may seem unrelated to atrial fibrillation.
- Write down key personal information, including any family history of Heart disease, stroke, high blood pressure or diabetes, and any major stresses or recent life changes.
- Make a list of all medications, vitamins, or supplements that you're taking.
- Take a family member or friend along, if possible. Sometimes it can be difficult to understand and remember all the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Your time with your doctor is limited, so preparing a list of questions will help you make the most of your time together. List your questions from most important to least important, in case time runs out. For atrial fibrillation, some basic questions to ask your doctor include:
- What is likely causing my symptoms or condition?
- What are other possible causes for my symptoms or condition?
- What kinds of tests will I need?
- What's the most appropriate treatment?
- What foods should I eat or avoid?
- What's an appropriate level of physical activity?
- How often should I be screened for Heart disease or other complications of atrial fibrillation?
- What are the alternatives to the primary approach that you're suggesting?
- I have other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a specialist? What will that cost, and will my insurance cover seeing a specialist? (You may need to ask your insurance provider directly for information about coverage.)
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend visiting?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may save time to go over any points you want to spend more time on. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
Tests and Diagnosis
To diagnose atrial fibrillation, your doctor may review your signs and symptoms, review your medical history, and conduct a physical examination. Your doctor may order several tests to diagnose your condition, including:
- Electrocardiogram (ECG). An ECG uses small sensors (electrodes) attached to your chest and arms to record electrical signals as they travel through your heart. This test is a primary tool for diagnosing atrial fibrillation.
- Holter monitor. This portable ECG device is carried in your pocket or worn on a belt or shoulder strap. It records your heart's activity for 24 hours or longer, which provides your doctor with a prolonged look at your heart rhythms.
- Event recorder. This portable ECG device is intended to monitor your heart activity over a few weeks to a few months. You activate it only when you experience symptoms of a fast heart rate.
- Echocardiogram. In this noninvasive test, sound waves are used to produce a video image of your heart. Sound waves are directed at your heart from a wand-like device (transducer) that's held on your chest (transthoracic echocardiogram). The sound waves that bounce off your heart are reflected through your chest wall and processed electronically to provide video images of your heart in motion, to detect underlying structural Heart disease.
- Blood tests. These help your doctor rule out thyroid problems or other substances in your blood that may lead to atrial fibrillation.
- Chest X-ray. X-ray images help your doctor see the condition of your lungs and heart. Your doctor can also use an X-ray to diagnose conditions other than atrial fibrillation that may explain your signs and symptoms.
Treatment and Drugs
The atrial fibrillation treatment that is most appropriate for you will depend on how long you've had atrial fibrillation, how bothersome your symptoms are, and the underlying cause of your atrial fibrillation. Generally, the treatment goals for atrial fibrillation are to:
- Reset the rhythm or control the rate
- Prevent blood clots
The strategy you and your doctor choose depends on many factors, including whether you have other problems with your heart and if you're able to take medications that can control your heart rhythm. In some cases, you may need a more invasive treatment, such as surgery or medical procedures using catheters.
In some people, a specific event or an underlying condition, such as a thyroid disorder, may trigger atrial fibrillation. Treating the condition causing atrial fibrillation may help relieve your heart rhythm problems. If your symptoms are bothersome or if this is your first episode of atrial fibrillation, your doctor may attempt to reset the rhythm.
Resetting your heart's rhythm
Ideally, to treat atrial fibrillation, the heart rate and rhythm are reset to normal. To correct your condition, doctors may be able to reset your heart to its regular rhythm (sinus rhythm) using a procedure called cardioversion, depending on the underlying cause of atrial fibrillation and how long you've had it. Cardioversion can be conducted in two ways:
- Electrical cardioversion. In this brief procedure, an electrical shock is delivered to your heart through paddles or patches placed on your chest. The Shock stops your heart's electrical activity momentarily. When your heart begins again, the hope is that it resumes its normal rhythm. The procedure is performed during sedation, so you shouldn't feel the Electric Shock.
- Cardioversion with drugs. This form of cardioversion uses medications called antiarrhythmics to help restore normal sinus rhythm. Depending on your heart condition, your doctor may recommend trying intravenous or oral medications to return your heart to a normal rhythm.
This is often done in the hospital with continuous monitoring of your heart rate. If your heart rhythm returns to normal, your doctor often will prescribe the same anti-arrhythmic medication or a similar one to try to prevent more spells of atrial fibrillation.
Before cardioversion, you may be given a blood-thinning medication such as warfarin (Coumadin) for several weeks to reduce the risk of blood clots and Stroke. Unless the episode of atrial fibrillation lasted less than 48 hours, you'll need to take warfarin for at least four weeks after cardioversion to prevent a blood clot from forming even after your heart is back in normal rhythm.
Or, instead of taking blood-thinning medications, you may have a test called transesophageal echocardiography — which can tell your doctor if you have any heart blood clots — just before cardioversion.
Maintaining a normal heart rhythm
After electrical cardioversion, your doctor may prescribe anti-arrhythmic medications to help prevent future episodes of atrial fibrillation. Medications may include:
- Dofetilide (Tikosyn)
- Flecainide
- Propafenone (Rythmol)
- Amiodarone (Cordarone, Pacerone)
Although these drugs may help maintain a normal heart rhythm, they can cause side effects, including:
- Nausea
- Dizziness
- Fatigue
Rarely, they may cause ventricular arrhythmias — life-threatening rhythm disturbances originating in the heart's lower chambers. These medications may be needed indefinitely. Even with medications, the chance of another episode of atrial fibrillation is high.
Heart rate control
You may be prescribed medications to control your heart rate and restore it to a normal rate. Heart rate control can be achieved through several medications.
The medication digoxin (Lanoxin) may control heart rate at rest, but not as well during activity. Most people require additional or alternative medications, such as calcium channel blockers or beta-blockers.
Beta-blockers may cause side effects such as worsening of Heart failure and Low blood pressure (hypotension). Calcium channel blockers can also cause side effects and may need to be avoided if you have Heart failure or low blood pressure.
Catheter and surgical procedures
Sometimes medications or cardioversion to control atrial fibrillation doesn't work. In those cases, your doctor may recommend a procedure to destroy the area of heart tissue that's causing the erratic electrical signals and restore your heart to a normal rhythm. These options can include:
- Catheter ablation. In many people who have atrial fibrillation and an otherwise normal heart, atrial fibrillation is caused by rapidly discharging triggers, or "hot spots." These hot spots are like abnormal pacemaker cells that fire so rapidly that the upper chambers of your heart quiver instead of beating efficiently.
In catheter ablation, a doctor inserts long, thin tubes (catheters) into your groin and guides them through blood vessels to your heart. Electrodes at the catheter tips can use radiofrequency energy, extreme cold (cryotherapy), or heat to destroy these hot spots, scarring the tissue so that the erratic signals are normalized. This corrects the arrhythmia without the need for medications or implantable devices.
- Surgical maze procedure. The maze procedure is conducted during open-heart surgery. Using a scalpel, doctors create several precise incisions in the upper chambers of your heart to create a pattern of scar tissue. Because scar tissue doesn't carry electricity, it interferes with stray electrical impulses that cause atrial fibrillation. Radiofrequency or cryotherapy also can be used to create scars, and there are several variations of the surgical maze technique.
These procedures have a high success rate, but atrial fibrillation may recur. Some people may need catheter ablation or other treatment if atrial fibrillation recurs.
Because the surgical maze procedure requires open-heart surgery, it's generally reserved for people who don't respond to other treatments or when it can be done during other necessary heart surgery, such as coronary artery bypass surgery or heart valve repair.
- Atrioventricular (AV) node ablation. If medications or other forms of catheter ablation don't work, or if you have side effects or are not a good candidate for other procedures, AV node ablation may be another option. The procedure involves applying radiofrequency energy to the pathway connecting the upper chambers (atria) and lower chambers (ventricles) of your heart (AV node) through a catheter to destroy this small area of tissue.
The procedure prevents the atria from sending electrical impulses to the ventricles. The atria continue to fibrillate, though. A pacemaker is then implanted to keep the ventricles beating properly. After AV node ablation, you'll need to continue to take blood-thinning medications to reduce the risk of stroke because your heart rhythm is still atrial fibrillation.
Preventing blood clots
Many people with atrial fibrillation or those who are undergoing certain treatments for atrial fibrillation are at especially high risk of blood clots that can lead to Stroke. The risk is even higher if another Heart disease is present along with atrial fibrillation. Your doctor may prescribe blood-thinning medications (anticoagulants) such as:
- Warfarin (Coumadin). Warfarin may be prescribed to prevent blood clots. If you're prescribed warfarin, carefully follow your doctor's instructions. Warfarin is a powerful medication that may cause dangerous bleeding. You'll need to have regular blood tests to monitor warfarin's effects.
- Newer anticoagulants. Several newer blood-thinning medications (anticoagulants) are available. These medications are shorter acting than warfarin and don't require monitoring. It's very important to take these medications exactly as prescribed. You shouldn't take the newer anticoagulants if you have a mechanical heart valve.
Dabigatran (Pradaxa) is an anticoagulant medication that's as effective as warfarin at preventing blood clots that can lead to Strokes and doesn't require blood tests to make sure you're getting the proper dose.
Rivaroxaban (Xarelto) is another anticoagulant medication that's as effective as warfarin for preventing Strokes. Rivaroxaban is a once-daily medication.
Apixaban (Eliquis) is another anticoagulant medication that's as effective as warfarin for preventing Strokes.
Talk to your doctor about taking one of these newer anticoagulants as an alternative to warfarin if you're concerned about your risk of Stroke. Follow your doctor's dosing instructions carefully and don't stop taking any of these medications without talking to your doctor first.
Many people have spells of atrial fibrillation and don't even know it — so you may need lifelong anticoagulants even after your rhythm has been restored to normal.
Lifestyle and Home Remedies
To prevent atrial fibrillation, it's important to live a heart-healthy lifestyle to reduce your risk of heart disease. A healthy lifestyle may include:
- Eating a heart-healthy diet
- Increasing your physical activity
- Avoiding smoking
- Keeping a healthy weight
- Limiting or avoiding caffeine and alcohol
- Reducing stress, as intense stress and anger can cause heart rhythm problems
- Use over-the-counter medications with caution, as some cold and cough medications contain stimulants that may trigger a rapid heartbeat.



